Maternal Mortality in the U.S.: A Growing Concern
admin April 23, 2025Science News ArticleMaternal mortality in the U.S. poses a serious public health challenge, as recent studies reveal a continued rise in pregnancy-related deaths across the nation. Alarmingly, over 80 percent of these fatalities are preventable, highlighting significant gaps in maternal health disparities, particularly among marginalized communities. The latest research conducted by the National Institutes of Health indicates that profound inequalities exist, with minority groups, such as American Indian and Alaska Native women, suffering the highest mortality rates. The COVID-19 pandemic exacerbated these issues, emphasizing the urgent need for improved prenatal care and extended postpartum support. As the nation grapples with these alarming statistics, it becomes imperative to address the systemic factors contributing to maternal health crises.
The stark reality of maternal mortality in the United States reflects grave concerns within women’s health, with rising rates of pregnancy-associated deaths generating critical dialogue around this pressing issue. Various factors, including insufficient access to quality prenatal and postpartum care, reveal deep-rooted healthcare inequities that predominantly affect women of color and those living in underserved areas. As we examine the broader context of maternal well-being, we must consider the challenges posed by the COVID-19 pandemic and its lasting impact on women’s health outcomes. Efforts to understand and reverse these trends are essential in the quest to ensure safe motherhood for all women. It is crucial to advocate for comprehensive strategies that prioritize maternal health and work towards eliminating disparities in care.
Understanding Maternal Mortality in the U.S.
Maternal mortality in the U.S. is a pressing public health concern, with the country experiencing higher rates of pregnancy-related deaths compared to its high-income peers. Over 80% of these deaths are recognized as preventable, highlighting critical gaps in healthcare systems. Factors contributing to this epidemic include a fragmented healthcare system, inadequate prenatal care access, and pronounced maternal health disparities, particularly across racial and ethnic lines. Current statistics reveal that American Indian and Alaska Native women face mortality rates almost four times greater than their white counterparts, indicating a need for targeted interventions.
Research findings from the National Institutes of Health underscore the urgent need for policy changes and improved healthcare delivery. The conversation surrounding maternal mortality must extend beyond the birth process itself to consider the entire continuum of care—from prenatal services and delivery to postpartum support. By recognizing that maternal health is not a finite issue limited to pregnancy, healthcare providers and policymakers can better address the chronic conditions that contribute to mortality, such as hypertension and cardiovascular diseases.
The Impact of COVID-19 on Maternal Health Disparities
The COVID-19 pandemic has significantly impacted maternal health, exacerbating existing disparities and highlighting the urgent need for improved maternal care. The pandemic prompted a rise in maternal mortality rates, particularly during the initial years when healthcare systems faced overwhelming demands. This disruption led many women to delay or forgo essential prenatal and postpartum care due to fear of exposure to the virus in healthcare settings. The implications of such delays have been dire, as gaps in care directly correlate with increased risks of complications and maternal mortality.
Furthermore, as the pandemic continues to influence healthcare practices, its effects on marginalized communities require immediate attention. Women of color have been disproportionately affected, with higher rates of pregnancy-related complications and deaths during this period. This reality highlights the necessity for healthcare systems to adapt and innovate in providing care that is both accessible and equitable. Strategies may include enhanced telehealth services, community-based support systems, and targeted outreach to at-risk populations to ensure comprehensive maternal health support during and beyond times of crisis.
The Role of Prenatal and Postpartum Care in Reducing Risks
Investing in quality prenatal and postpartum care is pivotal for reducing maternal mortality rates in the U.S. Studies show that timely access to prenatal care significantly lowers risks associated with pregnancy-related deaths. Expecting mothers need regular check-ups, screenings for chronic conditions, and educational resources to ensure a healthy pregnancy. By promoting maternal health education and equitable access to healthcare, we can empower women to seek care early, address potential health issues, and ultimately improve pregnancy outcomes.
Postpartum care is equally crucial, yet often overlooked in maternal health discussions. Many women experience complications well after delivery, emphasizing the importance of continued monitoring and support beyond the initial postpartum weeks. Policies must adapt to treat the postpartum period as a critical phase that extends up to a full year after childbirth. By reforming healthcare systems to provide comprehensive postpartum services, we can better prevent late maternal deaths and address women’s ongoing health needs following delivery.
Addressing Maternal Health Disparities in Racial Groups
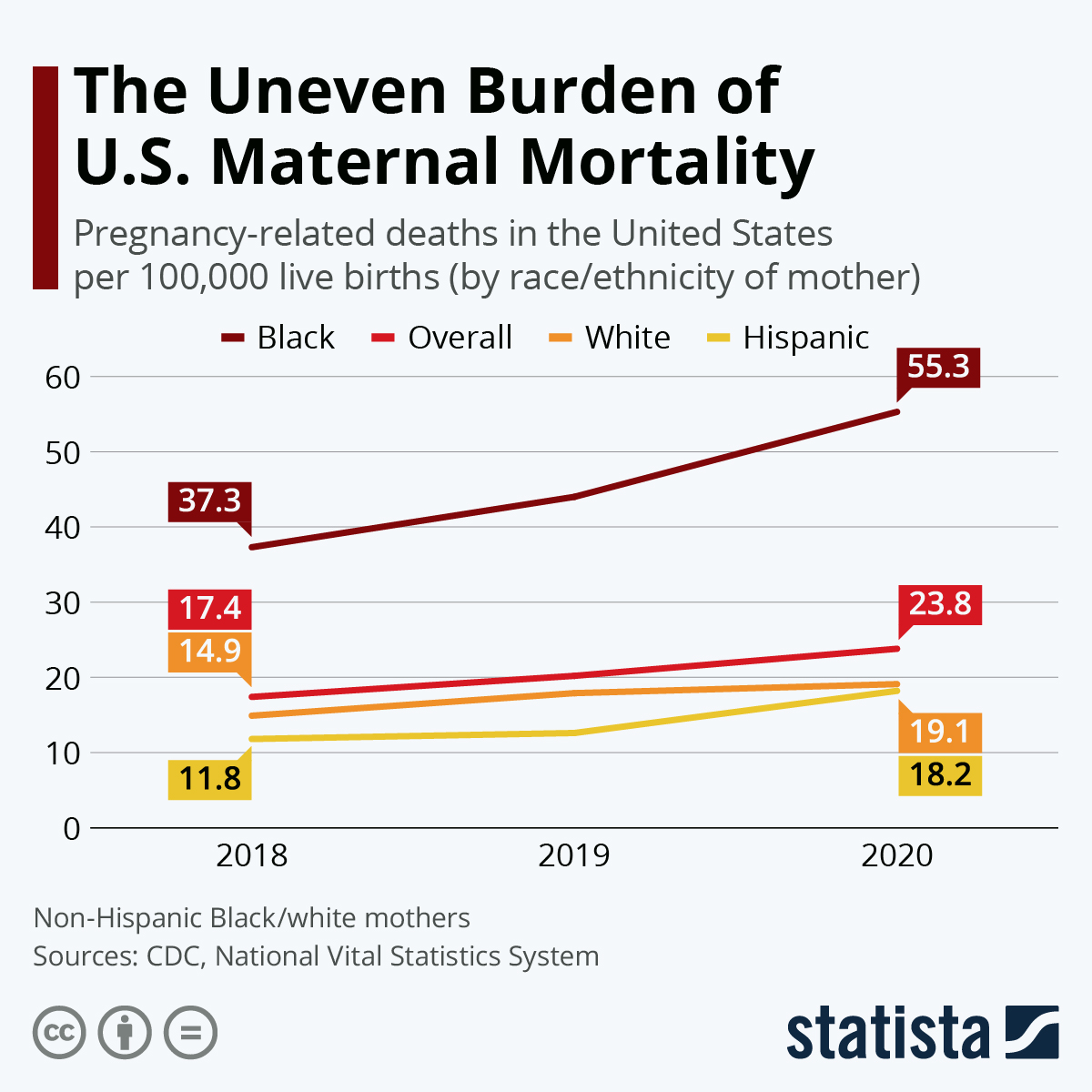
Maternal health disparities are starkly pronounced among various racial and ethnic groups in the United States. Recent data indicate that non-Hispanic Black and American Indian women experience significantly higher rates of pregnancy-related deaths compared to white women. These disparities are attributed to systemic issues within the healthcare system, including access to care, bias in treatment, and the prevalence of chronic health conditions. Addressing these disparities requires targeted policies that promote equity in maternal health resources and services, ensuring all women receive the care they need.”},{
Frequently Asked Questions
What is the current state of maternal mortality in the U.S.?
Maternal mortality in the U.S. remains a significant public health issue, with over 80% of pregnancy-related deaths deemed preventable. From 2018 to 2022, the U.S. has had the highest maternal mortality rate among high-income countries, which rose sharply during the COVID-19 pandemic. In 2022, there were 32.6 pregnancy-related deaths per 100,000 live births, an increase from 25.3 in 2018.
How do maternal health disparities affect pregnancy-related deaths?
Maternal health disparities play a crucial role in the rising maternal mortality rates in the U.S. Racial and ethnic groups face significant inequities, with American Indian and Alaska Native women experiencing the highest rates of pregnancy-related deaths. These disparities highlight the need for targeted interventions to improve maternal health outcomes across diverse populations.
What are the major causes of maternal mortality in the U.S.?
Cardiovascular disease is the leading cause of maternal mortality in the U.S., accounting for over 20% of pregnancy-related deaths. The shift from hemorrhage to cardiovascular concerns indicates a growing prevalence of chronic conditions like hypertension among pregnant individuals, particularly those aged 25 to 39.
What role does prenatal care play in reducing maternal mortality in the U.S.?
Prenatal care is vital for reducing maternal mortality as it helps in identifying and managing potential health issues before and during pregnancy. Improved access to timely and comprehensive prenatal care can significantly lower the risk of complications and pregnancy-related deaths.
How has COVID-19 impacted maternal health in the U.S.?
The COVID-19 pandemic has negatively impacted maternal health, leading to an increase in pregnancy-related deaths, particularly in 2021. Factors such as healthcare disruptions, increased stress, and higher prevalence of chronic conditions during pregnancy contributed to this rise.
Why are late maternal deaths significant in the context of maternal mortality?
Late maternal deaths, occurring between 42 days and one year after childbirth, accounted for nearly a third of pregnancy-related deaths in recent studies. Recognizing this period is crucial for improving postpartum care and addressing the long-term health needs of mothers.
What can be done to improve maternal health outcomes in the U.S.?
To improve maternal health outcomes, it’s essential to invest in public health infrastructure, enhance access to quality prenatal and postpartum care, address systemic inequities, and implement effective policies across states. Increasing awareness and research funding is also vital to combat rising maternal mortality rates.
What are maternity care deserts and how do they relate to maternal mortality?
Maternity care deserts refer to areas with limited access to maternal healthcare services. These deserts contribute to maternal mortality by restricting pregnant individuals’ access to necessary care, highlighting the need for policies that improve healthcare availability in underserved regions.
| Key Points |
|---|
| More than 80% of pregnancy-related deaths in the U.S. are preventable. |
| The U.S. has the highest maternal mortality rate among high-income countries, which continues to rise. |
| 2021 saw the sharpest increase in maternal mortality rates, likely due to the COVID-19 pandemic. |
| Significant disparities exist in mortality rates among racial groups; American Indian and Alaska Native women have the highest rates. |
| Cardiovascular disease is currently the leading cause of pregnancy-related deaths in the U.S. |
| ‘Late maternal deaths’ account for nearly a third of total mortality, indicating a need for extended postpartum care. |
| Investment in public health infrastructure is crucial to address and reduce maternal mortality rates. |
Summary
Maternal mortality in the U.S. is a pressing public health issue, highlighted by a recent study indicating that over 80% of these deaths could be prevented. As the nation grapples with the highest maternal mortality rates among wealthy countries, ongoing disparities across states and racial groups complicate the solution. Efforts to enhance prenatal and postpartum care are imperative, as is the commitment to public health funding to ensure equitable access to quality healthcare for all mothers.
You may also like
Archives
Calendar
| M | T | W | T | F | S | S |
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 8 | 9 | 10 | 11 | 12 | 13 | 14 |
| 15 | 16 | 17 | 18 | 19 | 20 | 21 |
| 22 | 23 | 24 | 25 | 26 | 27 | 28 |
| 29 | 30 | 31 | ||||