Health Research Funding: How Cuts Impact Patient Safety
admin May 6, 2025Science News ArticleHealth research funding plays an essential role in advancing medical studies and ensuring patient safety. As federal grants experience unprecedented cuts, the ramifications are profoundly felt within the medical research community. This disruption not only hinders the oversight provided by Institutional Review Boards (IRBs) but also raises serious concerns regarding clinical research ethics and the protection of participants involved in various studies. Without adequate funding, the ability to monitor and implement stringent safety measures becomes severely compromised, placing vulnerable individuals at risk. It is crucial to recognize that every reduction in health research funding threatens the very foundation of patient safety and the ethical standards that govern medical research.
Funding for healthcare studies is critical for nurturing innovations that protect participants in clinical trials. The landscape of research financing can significantly impact how institutions conduct scientific evaluations and uphold ethics in human subjects research. Various terms such as medical research grants or funding support systems reflect the vast network of financial resources essential for the advancement of healthcare studies. These financial backings not only facilitate essential oversight but also ensure that patient interests remain the top priority throughout the research process. The morality of clinical trials depends heavily on sustained support, which ultimately drives improvements in patient outcomes.
The Importance of Health Research Funding
Health research funding is crucial in advancing medical knowledge and ensuring patient safety. It allows researchers to conduct extensive studies that evaluate new drugs, treatments, and medical techniques under stringent ethical guidelines. Without adequate funding, the ability to maintain high standards of medical research diminishes, which can lead to lapses in oversight and patient protection. Moreover, these funds also contribute to the operational expenses of Institutional Review Boards (IRBs) that play an essential role in safeguarding the rights and welfare of human subjects involved in research.
The halt in health research funding, such as the significant cuts cited recently, disrupts not just individual studies but the entire framework of research oversight. Institutions rely on these funds to implement rigorous safety protocols and ethical standards to protect patients involved in clinical trials. If funding continues to be cut, it could lead to fewer studies progressing through necessary approvals and a slowdown in the introduction of innovative therapies, leaving patients without access to potentially life-saving treatments.
How IRB Oversight Ensures Medical Research Safety
Institutional Review Boards (IRBs) are essential for the protection of participants in medical research. They meticulously review every aspect of a study proposal — from informed consent to risk assessment — to ensure that all ethical considerations are met before participant recruitment begins. This oversight process helps mitigate potential risks associated with research; it not only guards the rights of participants but also ensures that the studies’ findings can be trusted. Effective IRB oversight is especially critical in multi-site studies, where coordinated efforts across hospitals and universities are necessary.
Moreover, IRBs also serve as educational resources, guiding researchers on ethical practices and compliance with federal regulations. A reliable IRB can provide clear checks and balances, fostering an environment of trust and accountability in clinical research settings. As the landscape of medical research evolves, the importance of robust IRB oversight becomes even more prominent, particularly in ensuring that patient safety remains a paramount concern.
Ethical Considerations in Clinical Research
Ethics in clinical research is of paramount importance, ensuring that human subjects are treated with dignity and respect. Ethical oversight is essential, especially when considering historical instances of unethical medical experimentation that led to severe consequences for individuals and populations. The establishment of strict ethical guidelines, enforced by IRBs and funded through health research initiatives, has been instrumental in building public trust over time. Historical events underscore the need for transparency and accountability in research practices.
Failing to adhere to ethical standards could lead to significant decreases in public participation in clinical trials, which are vital for advancing medical knowledge. Continuous funding is necessary to uphold these ethical standards, allowing researchers to conduct comprehensive reviews and updates to their methodologies and safeguarding the welfare of participants involved. As we move forward, prioritizing ethical conduct in clinical research will be critical in restoring confidence among potential participants.
The Impact of Funding Cuts on Research Progress
Funding cuts have devastating ripple effects on medical research. When financial resources dry up, innovative research projects risk stagnating, leading to delays in critical inquiries into new treatments and healthcare practices. The abrupt halt to research funding can stop studies midstream, leaving unanswered scientific questions and potentially harmful gaps in patient care. As seen recently with the stop-work order issued to Harvard’s SMART IRB, funding interruptions can prevent new clinical sites from joining existing studies, adversely affecting the trajectory of research progression.
Additionally, the limitations imposed by funding cuts can erode trust within communities who participate in research, fostering skepticism about the intentions and integrity of the research enterprises. When people feel that their safety and well-being are not prioritized — often due to financial constraints affecting the research — they may withdraw from participation altogether. Thus, maintaining and increasing health research funding is vital for sustaining the momentum of progress within the medical research field.
The Role of Patient Safety in Medical Research
Patient safety is a cornerstone of any successful medical research endeavor. It is the ethical obligation of researchers to ensure that participants are not exposed to unnecessary risks throughout the study. Research involving human subjects must be designed with patient safety at the forefront, ensuring thorough assessments are conducted under the watchful eye of IRBs. Their role in evaluating risks versus benefits is crucial in shaping the development of safe medical practices.
Protective measures must be in place to address any adverse events participants might face during research. This includes effective data monitoring, informed consent processes, and an accessible system for participants to voice concerns. A commitment to patient safety not only helps to generate reliable research outcomes but also preserves the integrity of the medical research community, enhancing the public’s trust in clinical trials and their outcomes.
Innovative Solutions in Clinical Research Amidst Funding Challenges
As funding cuts threaten the landscape of medical research, innovative solutions are essential in navigating these challenges. Collaborative research efforts and shared resources among institutions can help mitigate the financial impact of funding losses. By pooling resources and expertise, researchers can continue to engage in meaningful research while minimizing costs. Such collaborations harness the collective strength of multiple institutions and can lead to groundbreaking discoveries in health and medicine.
Additionally, embracing technology can streamline clinical research processes, making them more efficient and less expensive. Electronic data collection methods, telehealth consultations, and virtual patient engagement strategies can enhance participant experience while ensuring rigorous oversight. As research funding becomes scarcer, leveraging these technological advancements will be critical to maintaining momentum in clinical trials and ensuring patient safety and research integrity.
Building Trust in Medical Research Among Communities
Trust is a fundamental element in the relationship between research institutions and community members participating in studies. The history of medical experimentation has highlighted the need for transparency and ethical conduct to rebuild lost trust. Researchers must actively engage with communities to listen to their concerns, educate them about the research process, and demonstrate how their participation translates into tangible benefits. This mutual engagement can foster a collaborative atmosphere in medical research, allowing for a more inclusive and ethical approach.
Additionally, establishing open communication channels and providing continuous updates about ongoing studies can enhance community buy-in. Acknowledging the contributions of participants and addressing their fears surrounding research practices are essential steps in creating an environment that encourages participation. As funding cuts threaten research efforts, building trust within communities becomes increasingly important to ensure that necessary studies continue to receive the participant engagement they require.
The Future of Medical Research Funding
The outlook for medical research funding is critical for the health landscape of the future. As we face escalating challenges related to funding cuts, developing sustainable financing models will be essential. Advocating for increased public and private investment in health research is crucial in supporting not just clinical studies but the entire framework that underpins patient safety and ethical practices. This calls for stakeholders, including policymakers, academic institutions, and the broader community, to collaborate in advocating for resources and frameworks that prioritize health research.
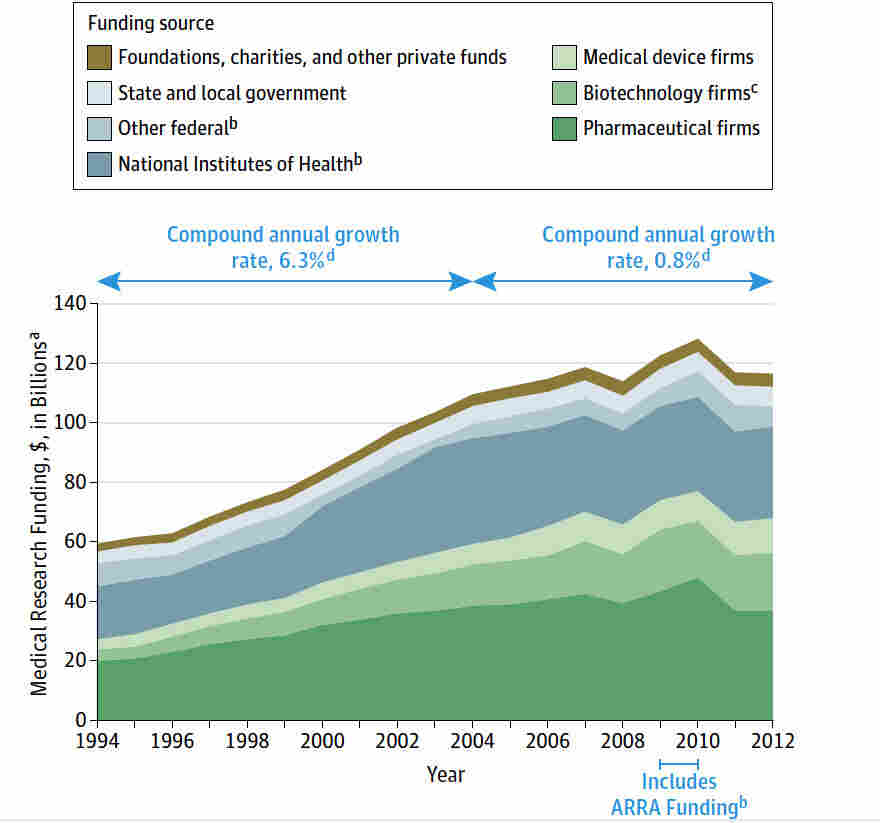
Moreover, as funding for health research remains in precarious conditions, diversifying funding sources — such as philanthropies, partnerships with private sector companies, and federal grants — can create a more robust backbone for medical innovation. By establishing a multi-faceted funding environment, medical research can continue to thrive and advance, ultimately leading to breakthroughs that enhance patient safety, improve health outcomes, and restore public trust in clinical research.
Collaborative Efforts for Enhanced Medical Oversight
Collaborative efforts among research institutions, governmental bodies, and the community are essential for enhancing oversight and implementing comprehensive patient safety measures. The establishment of partnerships focused on shared best practices can strengthen the integrity of clinical trials, ensuring they learn from past mistakes while navigating regulatory complexities. These collaborations can also influence the development of improved frameworks for ethical medical research, underscoring the importance of vigilance and accountability.
Moreover, community involvement in oversight processes can offer valuable insights and perspectives that may otherwise be overlooked. Engaging community members as active participants in shaping research ethics and practices ensures that studies are more reflective of the needs and expectations of the populations they aim to serve. By fostering these collaborative efforts, we can build a more ethical, transparent, and safety-oriented research environment that prioritizes patient welfare.
Frequently Asked Questions
How does health research funding ensure patient safety in clinical trials?
Health research funding, particularly from sources like the NIH, is crucial in facilitating the work of Institutional Review Boards (IRBs) that oversee clinical trials. These boards ensure compliance with ethical standards, safeguarding patient safety by reviewing research proposals, assessing risks, and verifying informed consent processes before studies can commence.
What impact do funding cuts have on the oversight of medical research safety?
Funding cuts for health research significantly disrupt the oversight mechanisms that IRBs provide. With reduced resources, institutions face challenges in maintaining rigorous safety protocols, potentially leading to risks for patients participating in clinical studies and undermining public trust in medical research.
What is the role of IRBs in protecting patients in health research funded studies?
IRBs play a vital role in health research funding by ensuring the rights and welfare of study participants. They evaluate the ethical aspects of research proposals, monitor ongoing studies, and ensure that participant safety is prioritized, thereby enhancing public confidence in clinical research.
How do changes in health research funding affect research ethics and patient safety?
Alterations in health research funding can compromise research ethics and patient safety by limiting the capacity of IRBs to effectively monitor studies. Insufficient funding may lead to inadequate oversight, increasing the risk of unethical practices and potential harm to participants.
What happens to clinical trials when health research funding is halted?
When health research funding is halted, many clinical trials face immediate disruptions, including the inability to start new sites or enroll participants. This can lead to delays in research timelines, increased risks for current participants, and may ultimately stifle advancements in patient safety and effective treatments.
Why is continuous funding vital for maintaining patient safety in health research?
Continuous health research funding is essential to ensure that robust systems are in place for monitoring patient safety. Funding supports the necessary infrastructure for IRBs, training of research staff, and implementation of effective oversight that guarantees ethical compliance and the welfare of participants.
How do historical events influence current standards in health research funding and ethics?
Historical abuses in medical research have shaped current standards in health research funding and ethics, emphasizing the importance of informed consent and rigorous oversight. These events led to the establishment of IRBs and the need for consistent funding to uphold patient safety and protect against past mistakes.
What is the SMART IRB initiative and its significance in health research funding?
The SMART IRB initiative streamlines the review process for multi-site health research funding by allowing a single IRB to oversee multiple sites. This efficient approach reduces bureaucratic barriers, ensuring patient safety while enhancing collaboration among researchers across various institutions.
| Key Points | Details |
|---|---|
| Funding Halt Impact | The Trump administration’s freeze of over $2 billion in federal research grants has stopped work on patient safety initiatives in medical research at Harvard. |
| SMART IRB Overview | SMART IRB is a system that facilitates oversight of multi-site medical research, ensuring patient rights and safety. |
| Role of IRBs | Institutional Review Boards (IRBs) safeguard patient welfare during research by reviewing proposals, ensuring informed consent, and mitigating risks. |
| Historical Significance | Past events, such as the Tuskegee Study and WWII experiments, highlight the importance of ethical oversight in medical research. |
| Consequences of Funding Cuts | Ongoing funding cuts lead to halted studies, increased risks for participants, and erosion of public trust in medical research. |
| Continued Efforts | Despite funding issues, Harvard Medical School continues to provide support for essential collaborative research efforts. |
Summary
Health research funding is essential for the ongoing protection and safety of patients involved in medical studies. The cuts in federal research grants not only disrupt vital oversight processes but also jeopardize public trust and the integrity of future research. Maintaining robust health research funding is crucial for ensuring that ethical standards in medical research are upheld.
You may also like
Archives
Calendar
| M | T | W | T | F | S | S |
|---|---|---|---|---|---|---|
| 1 | ||||||
| 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| 9 | 10 | 11 | 12 | 13 | 14 | 15 |
| 16 | 17 | 18 | 19 | 20 | 21 | 22 |
| 23 | 24 | 25 | 26 | 27 | 28 | |